Hot Seat #45 Denouement: 4yo F with edema
Posted on: October 23, 2014, by : Lenore Jarvis MD MEd
by Jason Woods, Children’s National
with Pavan Zaveri, Children’s National
The Case
4 year-old no PMHx p/w edema and a red rash involving bilateral eyelids as well as abdominal pain/distention and fatigue. Challenges of this case include what labs/imaging to obtain and who to consult in the setting of multi-organ involvement.
Here’s How You Answered Our Questions
The overall sentiment was that an ultrasound is needed to further delineate the abdominal distention/ascites, to look closely at the liver, and to rule out abdominal masses. Several fellows/attendings noted that if the abdominal ultrasound were negative, that they would consider an ECHO to look for a cardiac etiology.
Most felt that the patient could not be discharged home. Per Paul, look at the “ABCD” of the patient. If the patient was still tachycardic despite fluid boluses and continued to be weak, an admission is likely warranted. Also, remember to “close the loop.” If the PMD is not comfortable with outpatient follow-up, it is probably not appropriate to discharge the patient home. In this case, the patient had already been to the PMD several times prior to presentation to the ED.
Denouement
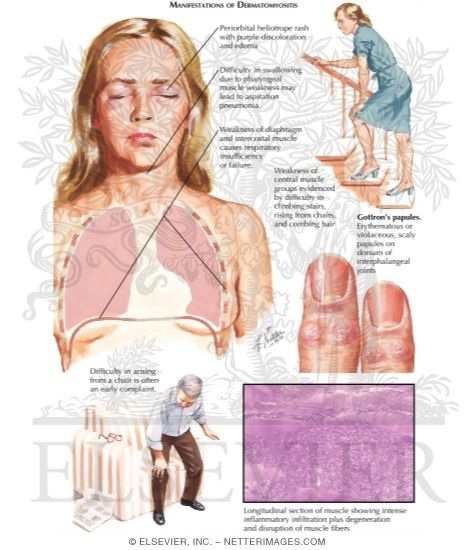
This patient was admitted to the hospitalist service with concern for a new onset inflammatory condition with consults by cardiology and rheumatology. Echocardiogram was negative. ANA titer 1:160 (positive). Rest of autoantibody panel returned negative. On HD 1-2 facial rash progressed into recognizable heliotrope rash. Based on heliotrope rash, proximal muscle weakness, and elevated inflammatory markers, he was given a preliminary diagnosis of Juvenile Dermatomyositis and started on an IV methylprednisolone burst, as well as IVIG x 2. On hospital day two he developed scaly, erythematous, blanching papules on bilateral knees, diagnoses as Gottron’s papules. MRI showed extensive inflammatory polymyositis, which was diagnostic for Dermatomyositis. Patient was discharged after 8 days on PO prednisolone with near resolution of symptoms.
Debrief Teaching Points – from Thursday Conference
Manifestations of Dermatomyositis: periorbital heliotrope rash, difficulty swallowing, weakness of the diaphragm, weakness of central muscle groups (difficult to arise from a chair), Gottron’s papules
Liver Tests: ALT/AST, bilirubin, ALP, albumin, total protein, GGT, PT, glucose
Consider – LDH, CMP, hepatitis testing, EtOH, ANA, drugs of abuse, copper, ceruloplasmin, AFP tumor markers, alpha-1 antitrypsin, acetaminophen, ammonia
Also “push on the liver” – if the HR increases, consider heart failure. If the heart rate decreases, the patient is likely dry.
Per Pavan, “going through all systems/processes like a med student (when so many systems are involved, breaking it down may help find the unifying diagnosis)”
Allergic, Cardiac, GI, Heme, Onc, Infectious, Neuro, Pulm, Renal, Rheum
