Orthopedics- Upper extremity #4 discussion
Posted on: April 15, 2019, by : Jennifer ChapmanJennifer Chapman, MD Children’s National Medical Center
This is a case of a 10yo child who injured his forearm after tripping. The Xrays show:


Your responses:
Respondents: 3 PEM fellows and 7 faculty, 1 PA
Is Orthopedic consult needed in ED:
Yes = 45 % No = 55%
Follow-up:
3-6 days: 18%
7-10 days: 55%
11-14 days: 18%
2-3 weeks: 9%
Diagnosis: SHII of the distal radius with angulation
Our Orthopedic colleague responds:
Clinical Pearls:
1. How is this a SHII?
To start with, the Xrays are inadequate: the AP and lateral are not sufficiently good to fully assess the fracture. One option is to obtain wrist films. These show the fracture extending to the physis from the metaphysis:


2. Salter-Harris classification refers to fractures involving the growth plate:
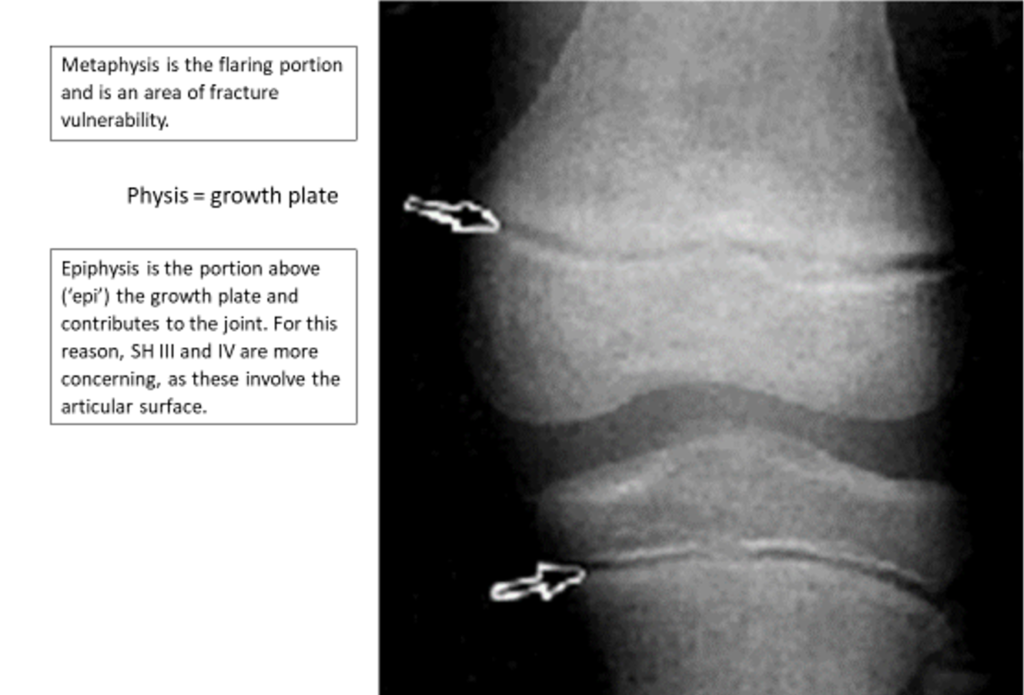
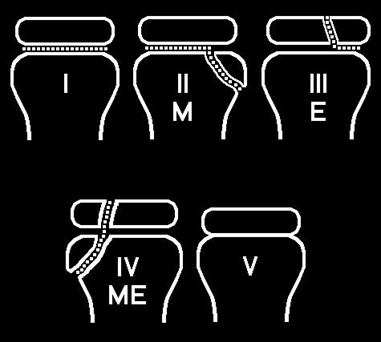
3. All growth plate fractures lead to some concern for growth arrest, though SH I and II fractures typically have good growth outcomes while the higher numbers are associated with higher rates of growth arrest. The good news is that, in the forearm, SH III and IV are rare. The broader concept is that the amount of energy contributing to a physeal fracture matters: in a femur physeal fracture, the energy required is higher and growth arrest is much more common, even for a SH I and II.
4. If there is angulation, early care is essential. Manipulation after 5 days may increase the rate of growth disturbance associated with physeal fractures.
5. Why is this fracture not a buckle? A buckle fracture is a pediatric-only pattern in which the more flexible bone can deform with an axial load. Differently from what we are often taught, a buckle fracture involves only one cortex and should therefore not angulate—this means that the metaphysis and shaft of the long bone remain straight, even if the cortex on one side is crumpled. If the long axis is angulated, then both cortices are involved and it is a transverse fracture.

Red flags requiring Orthopedic consult in the ED:
1. Angulation. There is a tool on our radiograph called ‘angle’ that allows you to draw 2 lines along the long axis of the bone and the bone distal to the fracture to describe an angle. An acceptable angle (one that does not require reduction) is deceptively complicated, as there are many considerations: age, distance from physis, rotational deformity, and degree. The general teaching is that a simple transverse fracture of the distal forearm with no involvement of the physis can be casted/splinted if it is less than 10 degrees in a child younger than 10 years. Our Orthopedic colleagues have a strong preference for early involvement for all angulated fractures, as these can move and be much more angulated at follow-up.
2. If the angulation of a distal forearm fracture is small (less than 10 degrees in a child under 10 years old), BUT the forearm looks deformed, this also is reason to reduce the fracture.*
*this is true at most academic institutions where the ED-ortho relationship is robust. There are other approaches possible when EDs have relationships with Orthopedic surgeons that allow scheduling of outpatient surgery soon after ED visit.
For this case, if the Orthopedist sees the child in the ED, follow-up would be in 7-10 days. If no consult and no cast (splint only), then the follow-up would be earlier- 3-6 days.
Pattern recognition: identify any injury

Case 2- Wrist AP













Xray readings:
Case 2: SHII of the distal radius with displacement. Really? Look at the lateral: the epiphysis is translated off the physis, and a small wedge of bone is separated off on the dorsal surface, making this a SHII.
Case 3: transverse fracture of the distal radius. The child was unable to follow-up for some months. Transverse fratures do have instability and can move in a splint. Follow-up films show a healing fracture now at 40 degrees of angulation. Because of the enormous capacity for remodeling over years, this healed to an improved angulation.
Case 4: transverse fracture of the distal radius. At 2-week follow-up, this fracture angulated to almost 30 degrees.
Case 5- a true buckle fracture of the distal radius
Case 6- SHII of the distal radius with displacement. If you can’t see a tiny triangle of bone extending from the metaphysis to the physis, then you might call this a SH I with displacement. Also ok, since either fracture would be recognized as requiring Orthopedic evaluation.
What remains unclear?